
FREE SHIPPING TO U.S. AND PUERTO RICO FOR ALL ORDERS $100 AND OVER!
We are unable to accept returns on any products or test kits. All sales are final.
By visiting our site, you agree to our privacy policy regarding cookies, tracking statistics, etc. Read more
FREE SHIPPING TO U.S. AND PUERTO RICO FOR ALL ORDERS $100 AND OVER!
We are unable to accept returns on any products or test kits. All sales are final.
FREE SHIPPING TO U.S. AND PUERTO RICO FOR ALL ORDERS $100 AND OVER!
We do not currently ship internationally.
Don’t guess, just test! Use our lab tests to assess core imbalances that can lead to many conditions. We test neurotransmitters, inflammation, hormones and much more. Purchase here and get started towards a healthier you today!
Shop from our pharmaceutical-grade, doctor-recommended, professional brands of natural health and brain supplements. Every item is carefully selected to guarantee quality ingredients and high-efficacy.
You’ve come to the right place. Integrative Psychiatry is making breakthroughs in treating this common and catastrophic epidemic, along with anxiety, ADHD, eating disorders and most other mental health conditions.
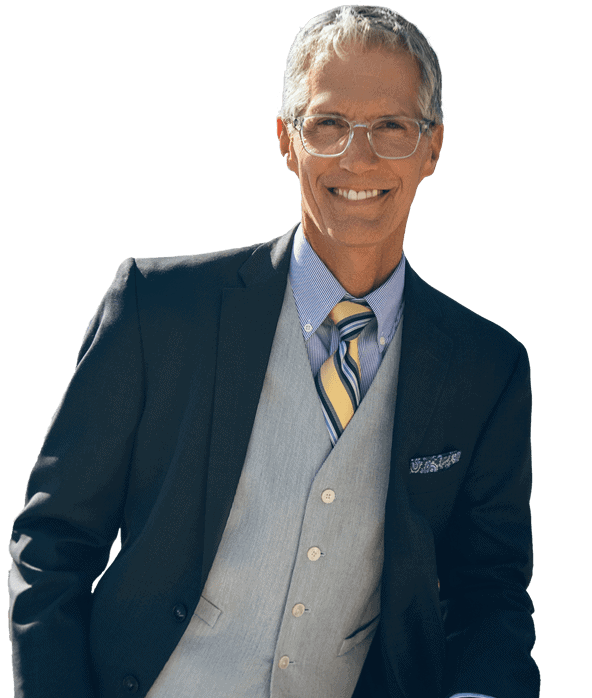
Integrative Psychiatry is a psychiatric and functional medicine practice located in Sarasota, Florida. Our practitioners offer a patient-centered model where we combine conventional medicine and evidence-based pharmaceutical treatments with complementary mind-body medicine, nutritional counseling, and preventative medicine to promote long term wellbeing. We strive to identify and treat the underlying causes and contributors to symptoms of depression, anxiety, brain fog, fatigue, obesity, insomnia, burnout, and other contemporary health conditions.
Achieving harmony between the brain and body is essential to whole body wellness. Our functional medicine approach identifies and treats core imbalances which affect your brain, body, and quality of life.
Treatment recommendations are based on a complete history, questionnaires and evaluations, targeted laboratory testing, and patient preference.













This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.